

Dr. Dan Galat is a board-certified orthopedic surgeon
who sub-specializes in total hip, knee, and shoulder
replacement surgery. Dr. Galat was fellowship trained
in Joint Replacement at the Mayo Clinic. He performs
surgery at Aloe Surgery Center Scottsdale. Dr. Galat is
in-network with most commercial carriers and welcomes
new Medicare patients in his Scottsdale office clinic.

Muscle sparing MAKO robotic assisted
total knee replacement

Muscle sparing MAKO robotic assisted partial
knee replacement

Minimally invasive ANTERIOR MAKO robotic
assisted total hip replacement

Minimally invasive

Education
Dr. Galat received his medical doctor’s degree at Ohio State University. He completed residency training and his fellowship in joint replacement at the Mayo Clinic; recognized as one of the highest quality and most prestigious institutions in the world, which trains only the very top applicants.
After finishing his residency training at the Mayo Clinic in Rochester, MN in 2008, he dedicated the first decade of his career to care for thousands of medically underserved patients in Kenya, East Africa, where he served at Tenwek Mission Hospital and Kijabe Medical Center. In 2019, he returned to Phoenix with his wife and 7 children to complete a one-year fellowship in Adult Reconstruction at the Mayo Clinic in Arizona. There, he trained extensively with experts in hip and knee MAKO robotic-assisted surgery and total shoulder arthroplasty, adding to his previous years of experience in Kenya.
Specialization
Dr. Galat is a leader in the field of robotic-assisted anterior total hip, total knee and partial knee replacement surgery. He brings his skill, compassion, and philosophy of healing to his Phoenix practice, Renovation Orthopaedics. Dr. Galat believes in holistic healthcare. Physical pain and disability from arthritis impacts a person emotionally, mentally, and spiritually. His goal is to repair and restore through personalized attention, and compassionate surgical care using cutting-edge technology, helping patients return to living their fullest life.
Dr. Galat performs the anterior approach for minimally invasivetotal hip replacement. The small incision for this approach is on the front of the hip by the groin. Patients can walk immediately after the procedure, which is done on an outpatient basis. By having outpatient surgery patients avoid the risk of Covid-19 and other hospital acquired infections, hospital errors, as well as higher risk of deep venous thrombosis. Recovery take 2-3 weeks; and best of all, once recovered, patients have no restrictions. The minimally invasive anterior total hip replacementapproach Dr. Galat performs incorporates the Stryker Mako robotic system. The two main advantages of Mako robotic hip replacement are 1) by creating a 3D computergenerated model of your hip from a CT scan the software assists Dr. Galat in picking the perfectly sized implants, that speeds recovery after total hip replacement and makes for a better long term outcome with less pain; and 2) the Mako robotic arms assists Dr. Galat in surgery, providing superhuman accuracy for making the cuts necessary for a snug fit for your implants.
Dr. Galat also performs a minimally invasive, tissue sparing total knee replacement using the Stryker Mako robot. The Mako total knee replacement robot assists Dr. Galat in picking the perfect sized implants, and to drill and make cuts with robotic accuracy.
Dr. Galant also performs total shoulder replacement. The efficacy of this procedure has greatly increased in recent years as surgeons have learned about the proper indications. In particular, people with end stage arthritis and rotator cuff tears require a reverse total shoulder replacement instead of the traditional anatomic total shoulder replacement.


You should do 3 weeks of physical therapy before considering an MRI—studies show worse results if you get imaging at this point. If you are not better after 3 weeks of therapy, then (6 weeks since the pan began) you should get an MRI and referral to a board-certified anesthesiologist or physiatrist with subspecialty certification and specialization in pain management. They will do a medial branch block and radiofrequency ablation as appropriate. Don’t let anyone talk you into epidural injection; that is not what you need.

You should do 3 weeks of physical therapy before considering an MRI—studies show worse results if you get imaging at this point. If you are not better after 3 weeks of therapy, then (6 weeks since the pan began) you should get an MRI. We can help you find a board-certified anesthesiologist or physiatrist with subspecialty certification and specialization in pain management who doesn’t over-prescribe dangerous narcotics.
They will offer you medial branch block and epidural injection. Those don’t really work for this problem. Your options are (off label) intradiscal injection of stem cell-derived growth factors, denervation with the relevant procedure, and then referral to a spine surgeon for interbody fusion if those fail.
You need an MRI now and referral to a spine surgeon for possible laminectomy decompression surgery. We can help you find one who is board-certified and specializes in minimally invasive surgery.
You need an MRI now and referral to a board-certified anesthesiologist or physiatrist with subspecialty certification and specialization in pain management. Don’t go to one that prescribes a lot of narcotics, they may get you killed. If you’re not better after 3 epidural injection you will be referred at 12 weeks to a spine surgeon to consider microdiscectomy. Note that you DO NOT need radiofrequency ablation; so, don’t let anyone talk you into a medial branch block.

This stuff can be confusing. Don’t sweat it. We’ve got you. Your MRI came with a report by a radiologist which describes the findings. If you don’t have a copy of your report, you can get one from the imaging center where the x-ray was taken. The doctor who prescribed the MRI has a copy as well. Find the section labeled Impression. First, under the impression, look for the word normal. If you see something like “Normal MRI of the hip then you are done. You do not need to check anything.
Next, search the impression section for the words osteonecrosis or avascular necrosis. If you see either one in the report, then ignore the rest of the report and check the osteonecrosis box. If neither of those is in the report, ignore the rest for now and continue.
This stuff can be confusing. Don’t sweat it. We’ve got you. Your x-ray came with a report by a radiologist which describes the findings. If you don’t have a copy of your report, you can get one from the imaging center where the x-ray was taken. The doctor who prescribed the x-ray has a copy as well. Find the section labeled Impression.

First, under the impression, look for the word normal. If you see something like “Normal x-ray of the hip then you are done. Check the box normal. Next, search the impression section for the word hypoplasia. If you see hypoplasia in the report then ignore the rest, and check the hypoplasia box.
If you are still going, then look for the word arthritis. The radiologist should have given the arthritis a grade from 1 to 4. If you see arthritis in the impression section but there is no grade, then look at the rest of the report for a grade 1,2,3 or 4 and check the appropriate box. If there’s no grade then you have every right to call the imaging center and ask them to have the radiologist to do their job and redo the report with a grade.

Not all orthopedic surgeons are the same. You deserve the best. That means a surgeon who is
In my experience less than 10% of orthopedic surgeons meet all five of these criteria. That means if you go to the surgeon you’ve been seeing, or the one recommended by friends or family, there’s a 90% chance you will not be getting the best.
At Phoenix Spine and Joint we make it our business to know the best. Call us for help finding the best surgeon near you who takes your insurance and is accepting new patients.

If you have any of the following red flags you need to see a doctor NOW!
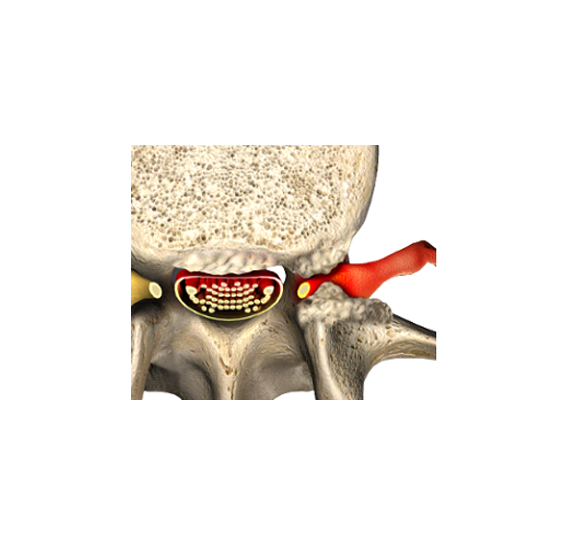
Radiculopathy. This condition is most often due to herniated disc, but can also be caused by bone spurs, or compression of nerve roots as they leave the spinal canal. The traditional treatment is to confirm the herniation or compression by MRI, followed by a trial of epidural injection, with microdiscectomy or laminectomy surgery if all else fails.
Enter below and we will email or text you more information about how to get rid of your radiculopathy due to herniated disc.

Facet syndrome. Your low back pain is most consistent with arthritis. Look for confirmation on your x-ray and MRI reports with discussion about “arthritis.” The traditional treatment is radiofrequency ablation done by a pain management physician.
Enter below and we will email or text you more information about how to get rid of your low back pain due to arthritis.

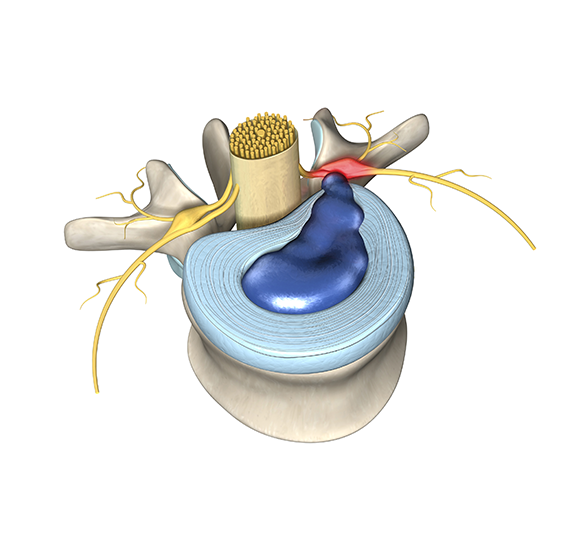
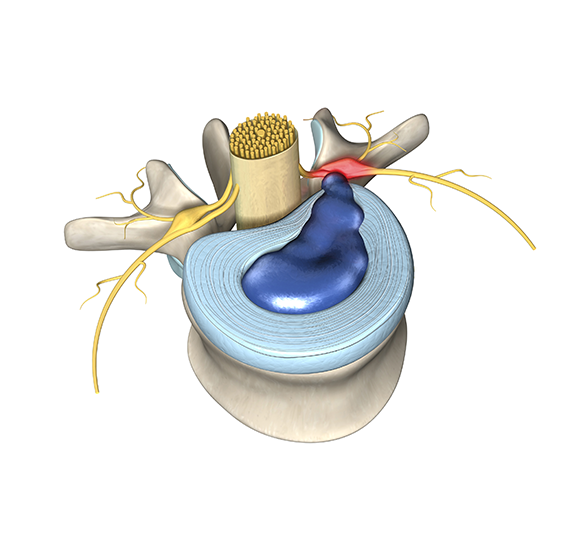
Discogenic low back pain due to an annular tear. Sorry, this is the least common and the hardest to treat. Traditionally, the recommended procedure is fusion; however, that does not always work and causes adjacent level issues. More recently a denervation procedure was approved called the Intercept procedure from Relievant. Some doctors recommend injection, The two options are stem cell-derived growth factors, and ozone.
Enter below and we will email or text you more information about how to get rid of your discogenic low back pain.

 Subscribe!
Subscribe!