When should I get an MRI of my low back
When should I get an MRI of my low back https://bestpracticehealth.tv/wp-content/uploads/2022/04/Layer-1aaa-1024x535.png 1024 535 Best Practice Health TV https://bestpracticehealth.tv/wp-content/uploads/2022/04/Layer-1aaa-1024x535.pngWhen should I get an MRI of my low back?
MRI (Magnetic resonance imaging) plays an especially vital role in helping your doctor know how to get rid of your low back pain. However, studies show getting an MRI too soon can lead to a bad result. So, when should you get an MRI of your low back?
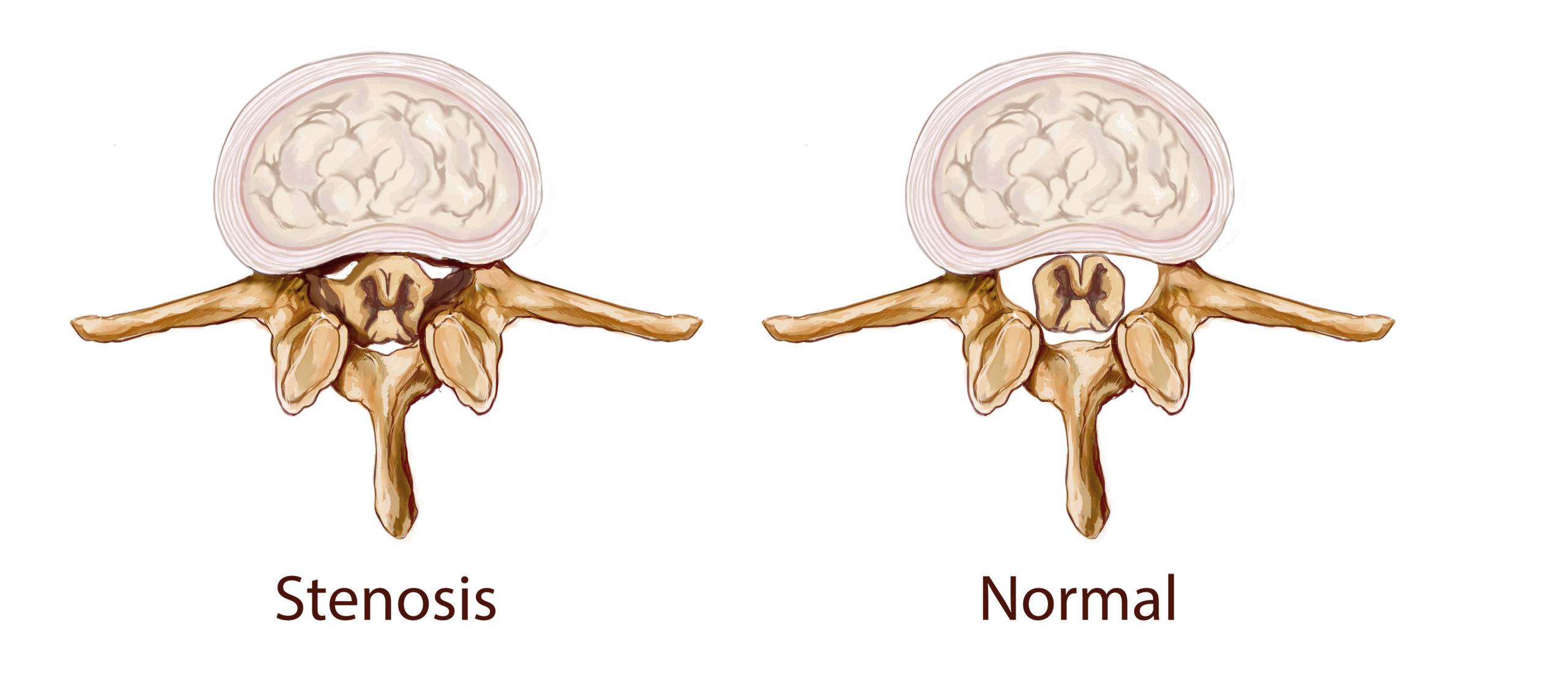
Most people with low back pain have arthritis, compression fracture, a torn disc, herniated disc, or spinal stenosis (narrowing). Arthritis and compression fractures show up on x-ray, but it takes MRI to know if you have a torn disc, herniated disc, or spinal stenosis. Your doctor will need to know which problem is present to recommend the right treatment plan. If you have red flags suggesting a serious underlying problem, you need an MRI and doctor visit emergently, which means right away.
But for most people, MRI should wait. The right time to get an MRI of your low back depends on how long your back has been hurting and the type of pain you experience.
To determine if you need an MRI of your back, you must know which of the five types of low back pain you have. Read to the end to learn to identify your pain and whether you need an MRI.
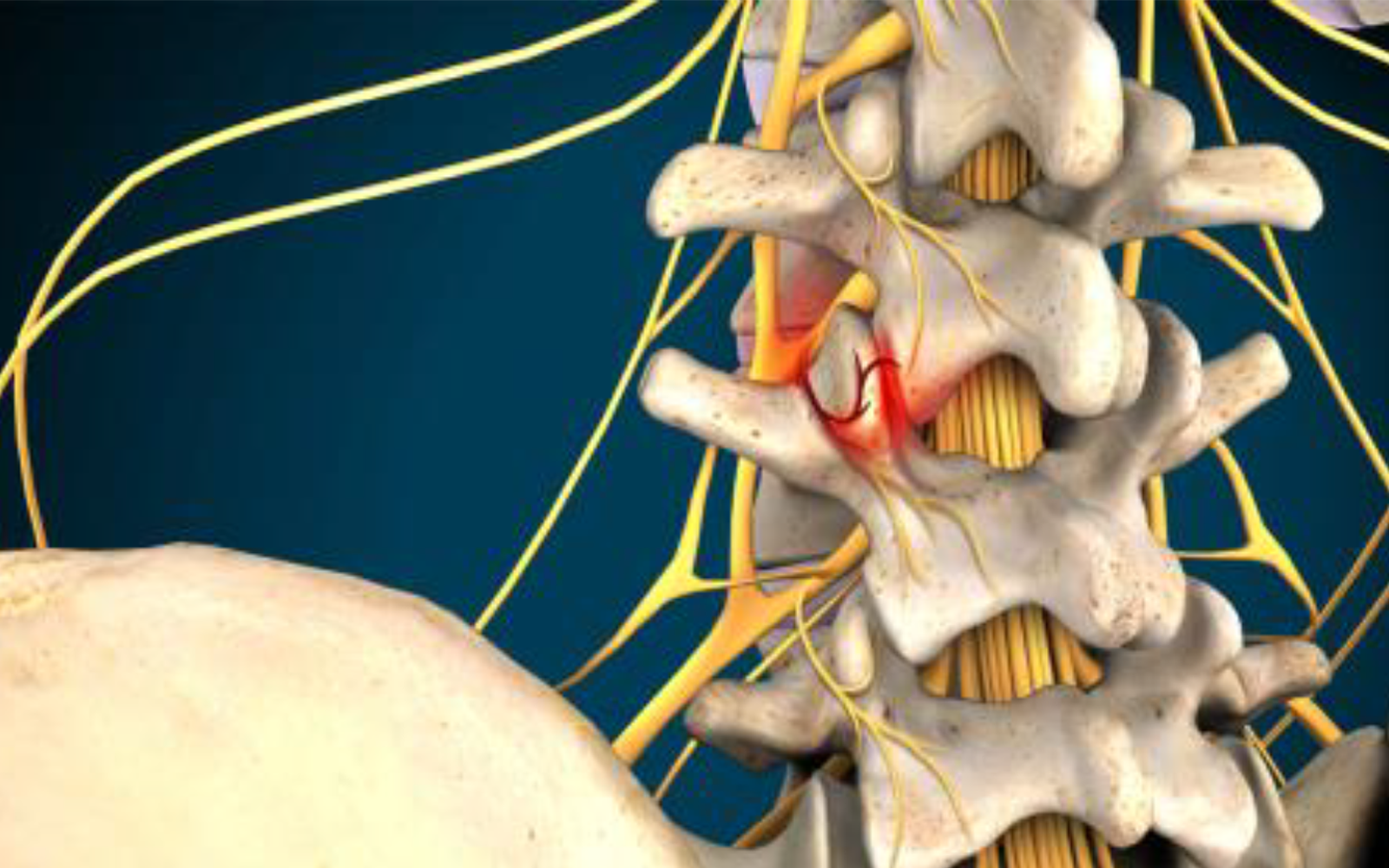
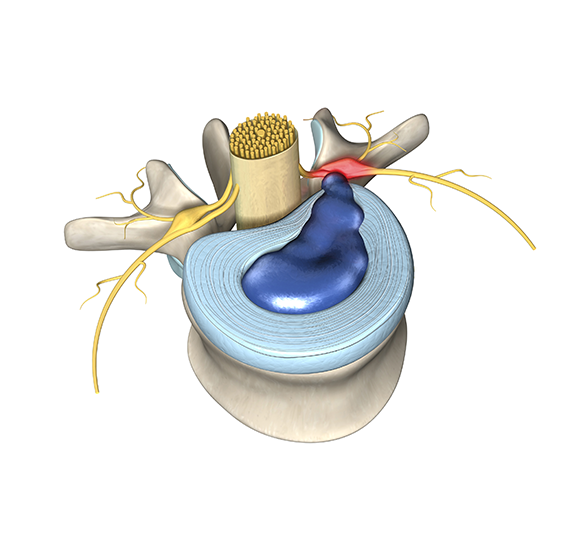
Your low back comprises five cube-shaped vertebral body bones separated by rubbery discs. Behind the bones, your spine forms a canal to contain and protect your nerve roots. Two facet joints connect each bone, one on each side, to the bones above and below —except the fifth
lumbar bone, which connects to your tailbone by two facet joints.
#1. Facet joint pain.
When a facet joint hurts, it causes a very unusual pattern. The pain from an inflamed or arthritic facet joint starts on the side of your low back and spreads into your butt. Facet joint pain often feels like it’s in your hip. If the pain gets bad, it burns in your outer thigh but does not typically go below the knee. Facet joint pain is caused by movement, so it feels better in a back brace.
#2. Knife in the back
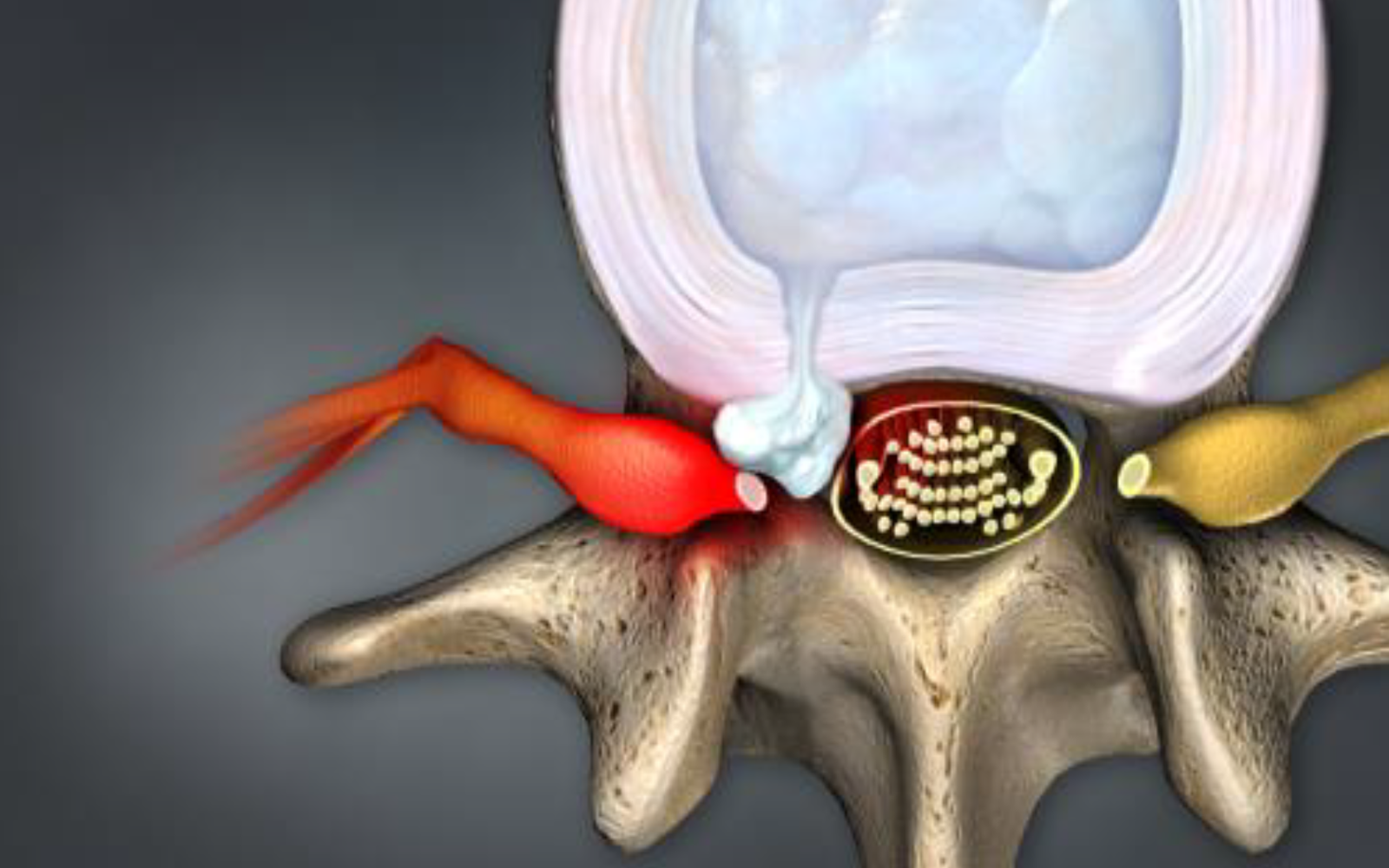
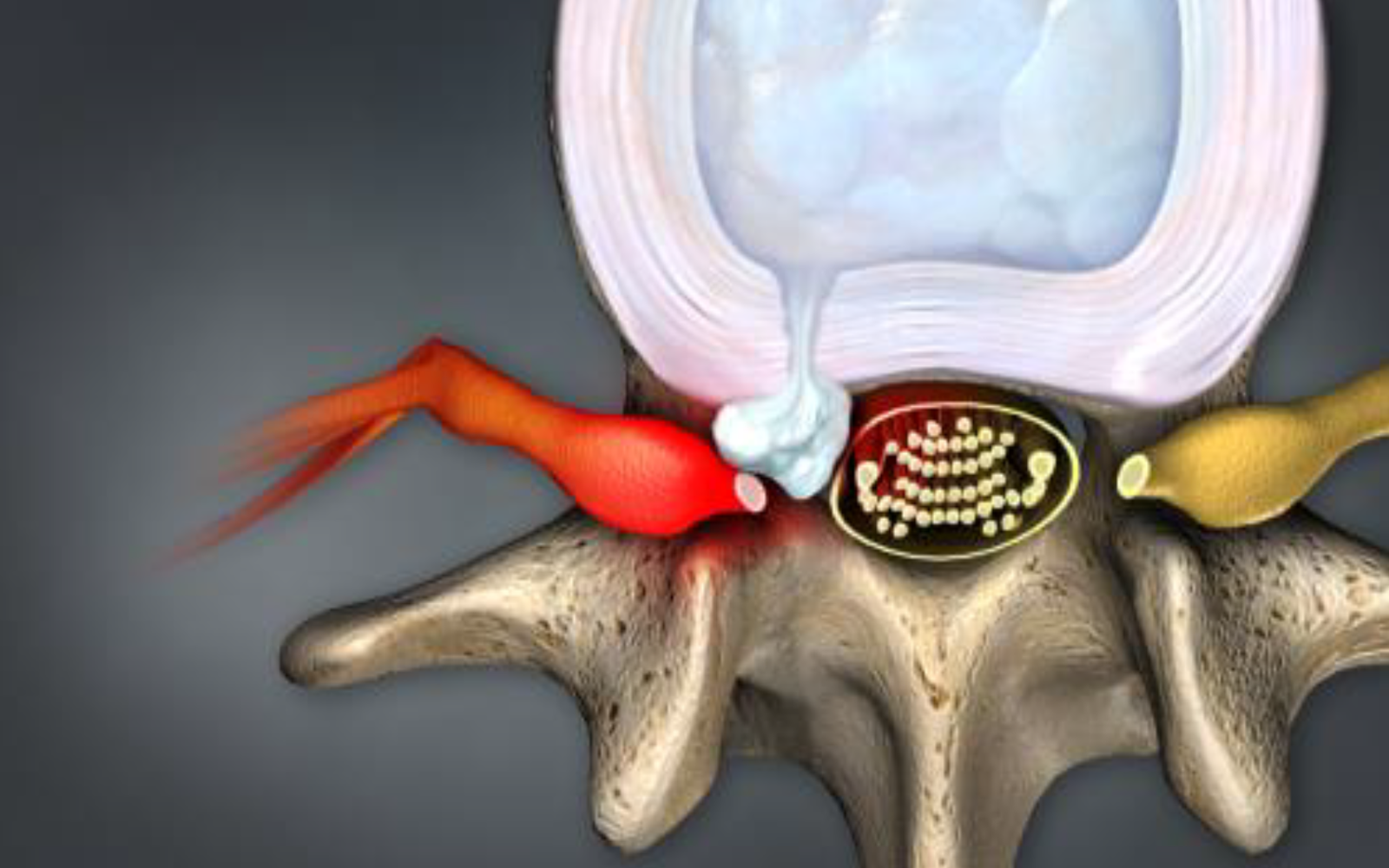
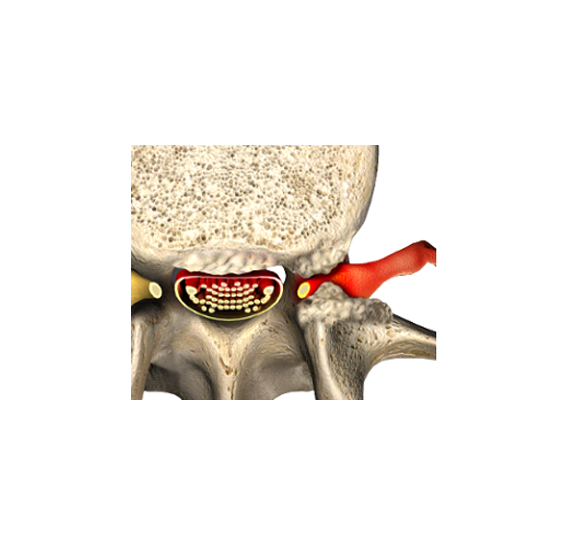
The discs that separate the spinal bones have two parts. The outer part is tough and made from tissue rings that look like the trunk of a tree cut on end. The inner part is soft and serves as a cushion.
An annular tear or compression fracture feels like a knife in the back. The pain is typically near the middle of your back and made worse by standing or even sitting. Unlike a painful facet, the pain from an annular tear or compression fracture does not typically radiate out from your back; it’s not in the hip and does not cause burning on the side of your thighs.
#3. Nerve root pain.
Inflamed nerve roots cause pain that starts in your back and shoots down your leg like electricity. Nerve root pain is typically associated with numbness and possibly weakness in the connected part of your leg. Unlike the back pain from a torn disc or compression fracture, nerve root pain does not feel like a knife in the middle of your back as it does radiate down your leg. The severe part of nerve root pain is not in your back; it’s the leg. Unlike facet pain which radiates to the outside of the thigh, nerve root pain typically crosses to the inside of the thigh and may go to your pinky toe, big toe, or inner ankle. People often call nerve root pain sciatica.
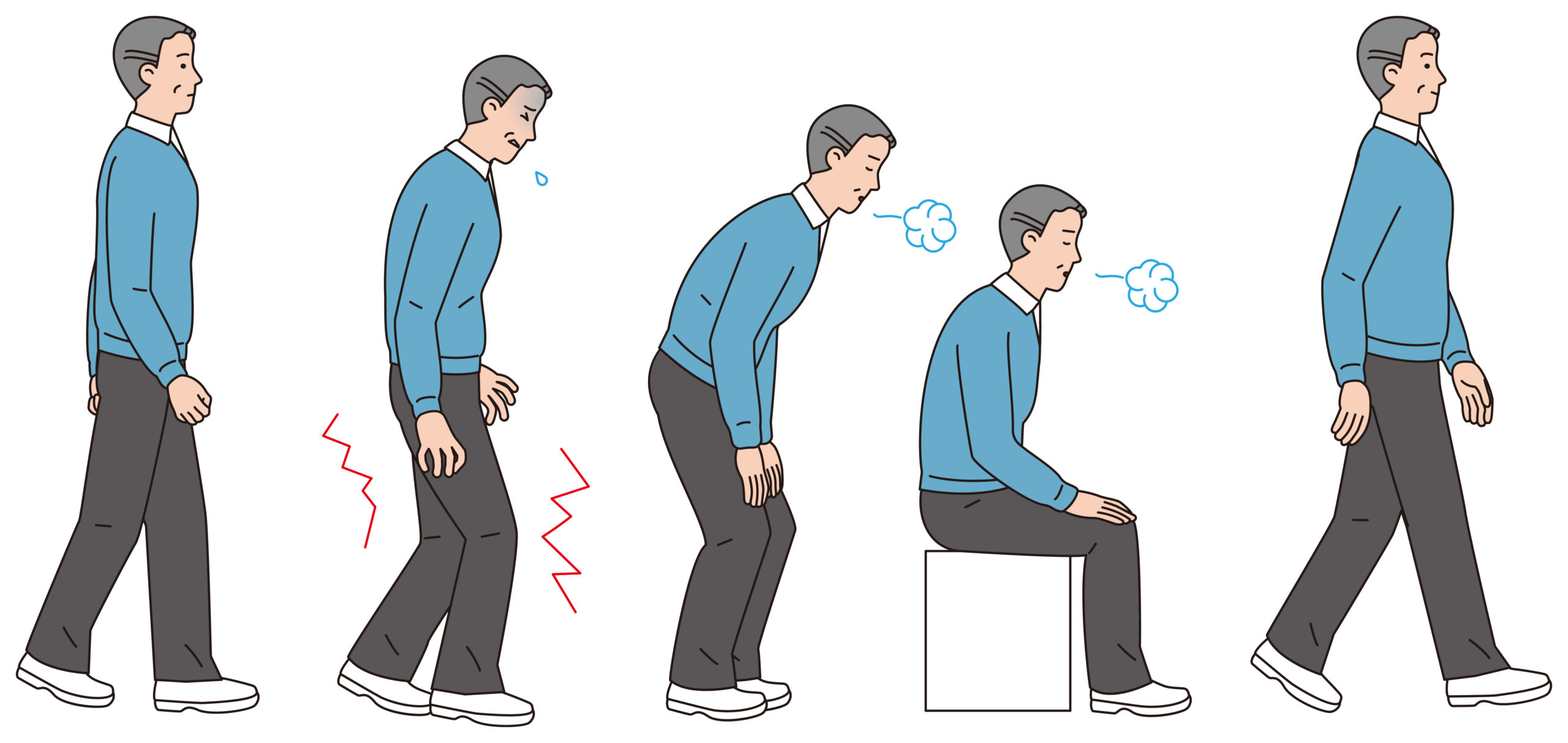
#4. Claudication
Back pain almost always (94%) goes away by itself without treatment in twelve weeks. However, some serious conditions require immediate evaluation. Knowing if you have a serious condition is by searching for red flags for back pain and consulting a physician.
Whew! That’s a lot of pain. But it was worth reviewing because now we know YOU NEED AN MRI OF YOUR BACK IF YOU HAVE:
- Facet joint pain for twelve weeks not relieved by conservative measures like moist heat (NSAIDs), non-steroidal anti-inflammatory drugs, a back support brace, and chiropractic treatment or physical therapy. Most people will wait for three weeks to see their doctor, get an x-ray, then start physical therapy. Ninety-four percent of people with facet pain are better in 12 weeks. If not, an MRI is needed.
- Knife in the back pain. A torn disc or compression fracture usually causes this type of pain. Your doctor will want you to get an x-ray right away for back pain following an accident as compression fractures show up nicely on an x-ray, and MRI may not be needed. Otherwise, your knife in the back pain persists after 12 weeks despite conservative measures, then MRI is needed.
- Nerve root pain for three weeks. A herniated disc causes most nerve root pain; however, bone spurs can also cause it. MRI should be obtained after three weeks as an epidural injection could help.
- Claudication. Spinal stenosis is a progressive condition that ends with urinary incontinence and paralysis followed by death in bed due to urinary tract infection. Luckily, this process is progressive but very slow. An MRI is needed to assess the degree of stenosis and ensure the claudication is coming from compressed nerve roots and not poor blood supply to the legs.
We know this is complicated. If you have any questions or comments we’re available in the chat box below or by phone at (602) 256-2525.