When should I get MRI (Magnetic Resonance Imaging) of my lumbar spine?
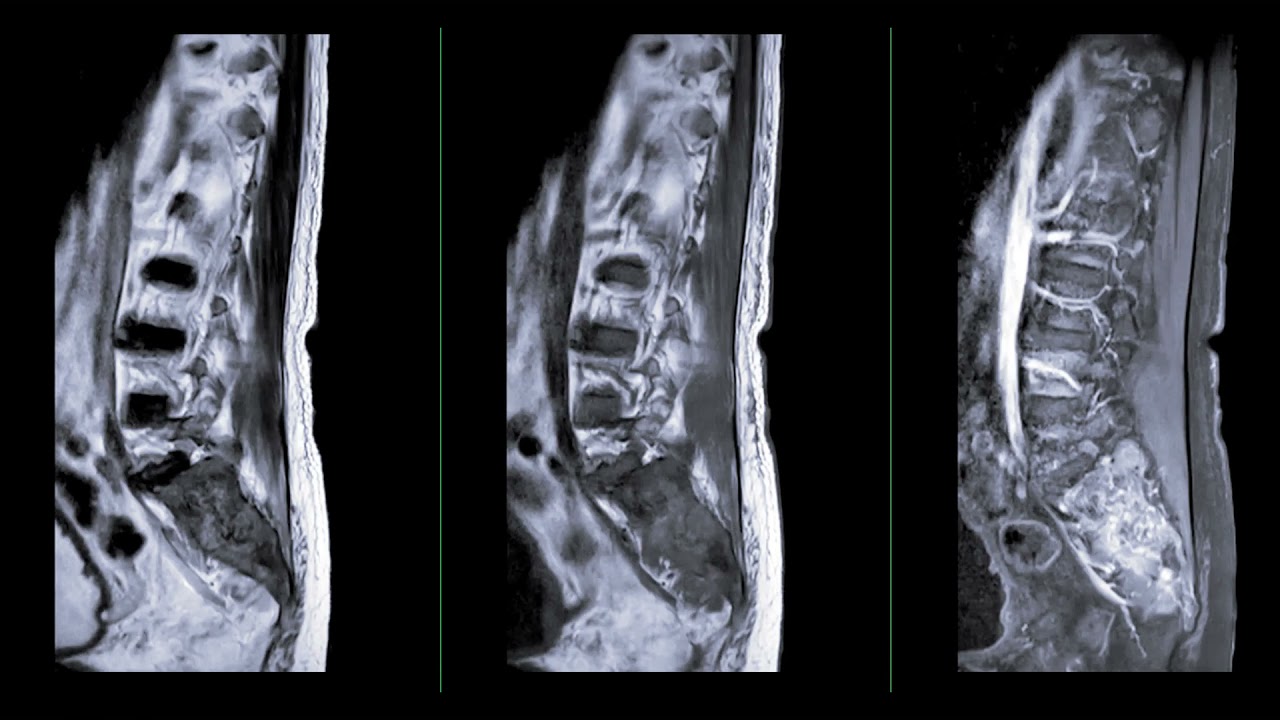
When should I get MRI (Magnetic Resonance Imaging) of my lumbar spine? https://bestpracticehealth.tv/wp-content/uploads/2023/10/Magnetic-Resonance-Imaging-Img-1024x285.png 1024 285 Best Practice Health TV Best Practice Health TV https://bestpracticehealth.tv/wp-content/uploads/2023/10/Magnetic-Resonance-Imaging-Img-1024x285.pngAs a soldier and single mother of 2 the last thing Sylvia Delgado needed was back pain. But that is what she developed after working out with heavy loads in the gym. A year later Sylvia’s pain was getting worse, she had not seen a specialist, or had any meaningful treatment other than physical therapy. She contacted me for help getting a treatment plan and to find out if there was hope for her to stay in the Army and be able to take proper care of her young daughter with autism.
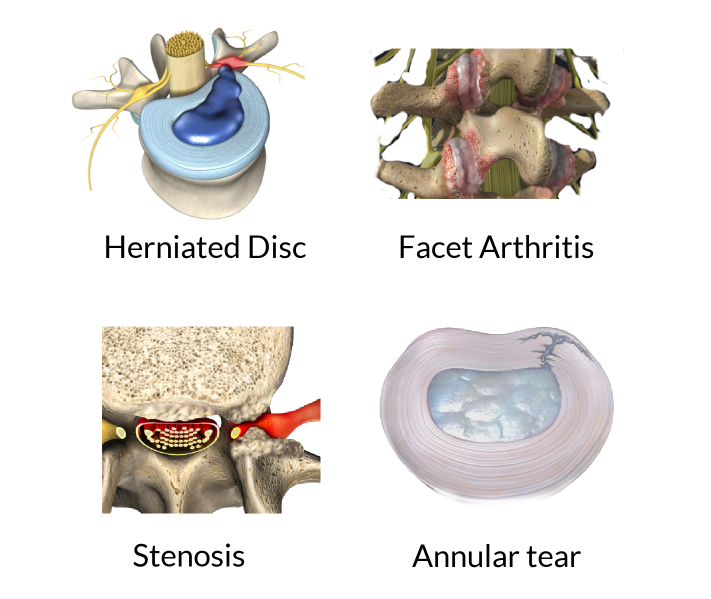
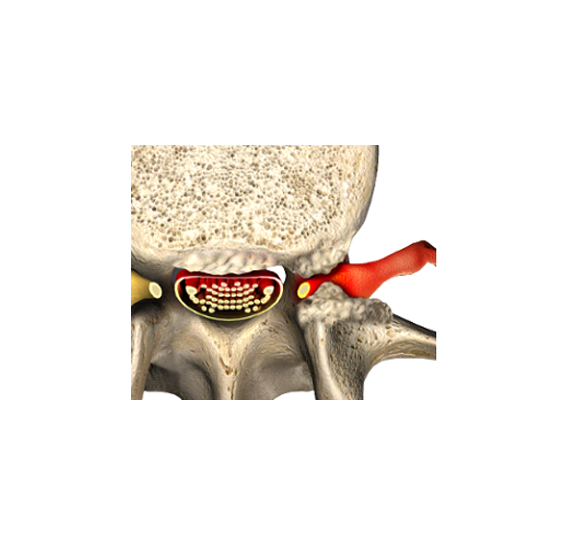
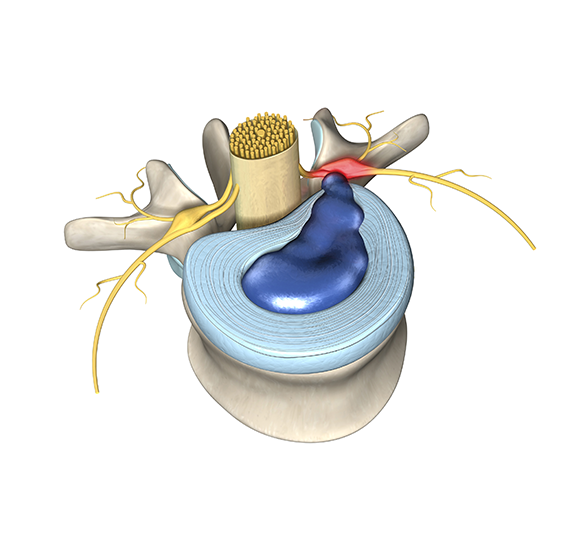
The four most common structural causes of non-specific low back pain are herniated disc, facet arthritis, spinal stenosis, and an annular tear. Herniated discs typically cause sciatica which is an electric pain that goes down the buttocks and into the leg, often associated with numbness and weakness. Facet pain is mostly in the butt off to the side, and radiates to the butt, feels like it is in the hip, and burns in the outer thigh. Stenosis causes a claudication pain that shoots down the legs with walking and is relieved by bending forward.
Other than muscle strains, there are 4 common causes of low back pain in the lumbar spine. Sylvia’s medical history and physical examination are notable for back pain that feels a red-hot needle which came on slowly after an injury and is worsening without signs of nerve damage. Of note, Sylvia does not have leg pain, weakness, or numbness below the waist. This pain pattern is typical of an annular tear. Disc material is made from soft cartilage, so internal disc disruption of this type will not show up on an x-ray. The definitive test to show if Sylvia has an annular tear is MRI (magnetic resonance imaging).
When Sylvia asked for an MRI her health care provider denied the request. Sylvia’s experience is typical of many non-soldiers as well. We all know insurance companies do not love to spend money. But why so much resistance to MRI of the low back? There are two reasons.
Over ninety percent of people with non-specific low back like Sylvia get better on their own in 6-12 weeks without treatment. Since they get better anyway, from the point of view of finding the right treatment, money spent on MRI is wasted. OK, but unlike other forms of diagnostic imaging— like X-ray and CT (Computed Tomography) — an MRI scan has no radiation, so there is no harm, right? In addition, MRI is a noninvasive procedure that involves simple radio wave energy. Why not just get an MRI anyway for peace of mind? Well, that’s not what science says.
Studies have shown patients who get MRI earlier in the course of non-specific low back pain do worse. And that makes sense. MRI shows structure not pain. Most people without low back pain have underlying spinal degeneration, even old traumatic injuries, or disc degeneration, that make abnormal low back MRI. That means if you get an MRI when you have pain, there’s no guarantee the things the radiology report describes are actually causing anything. That degree of false-positive results can lead to unnecessary treatment, and even complications.
In addition, not everyone can have one. MRI requires your entire body to be placed in a strong magnet that generates pulses of radio waves. Depending on your condition, the magnetic field may not be safe for those with certain types of metal implants, particularly electronics like pacemakers or loose metal objects. Even pigments in tattoos can be problematic if they contain metals. In rare cases MRI of the lumbar spine needs to be performed with gadolinium contrast which is not safe for people with kidney failure.
Nevertheless, based on your medical history, physical examination, and other diagnostic imaging studies (like x-ray or CT) there are medical conditions that demand the need for an MRI. You need a MRI imaging test for your lumbar spine right away if you check yes to any of the following:
- Radiating pain that is severe and may be associated with nerve root damage is sciatica. Detailed images are required to determine if you have a herniated disc. Sciatica in both legs, especially with bladder retention, may be cauda equina syndrome, a surgical emergency.
- Recent trauma or injury that is suspicious for a structural problem that may require you to act.
- Mechanical back pian and no improvement with conservative measure like rest, pain relievers (anti – inflammatories), and physical therapy after 6-12 weeks.
By the time she contacted me Sylvia had gone through weeks of home care, pain relievers like non-steroidal anti – inflammatories, and physical therapy. Her medical history strongly suggests an annular tear which often leads to herniated discs which do not show up in diagnostic studies like X-ray or CT. So, clearly MRI of the lumbar spine is Sylvia’s next step.
Stay tuned to find out what is next for Sylvia. If you need help figuring out the best treatment for your low back pain submit your questions by video at BestPracticeHealth.TV.
Watch my whole interview with Sylvia here: Seven months of low back pain, why won’t my doctor order an MRI? | Non-specific low back pain
Learn more about how MRI scans are performed, including how the test is performed, and how to prepare for the test here: Lumbar MRI scan: MedlinePlus Medical Encyclopedia
For an excellent review of whether you really need an MRI check this: Low Back Pain: Should I Have an MRI? | Kaiser Permanente

Dan Lieberman, MD
- Posted In:
- Knowledge Center